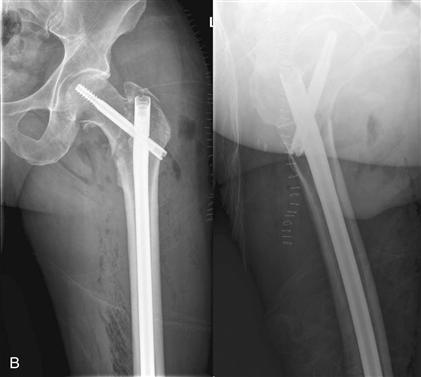
complete comminuted intertrochanteric fracture
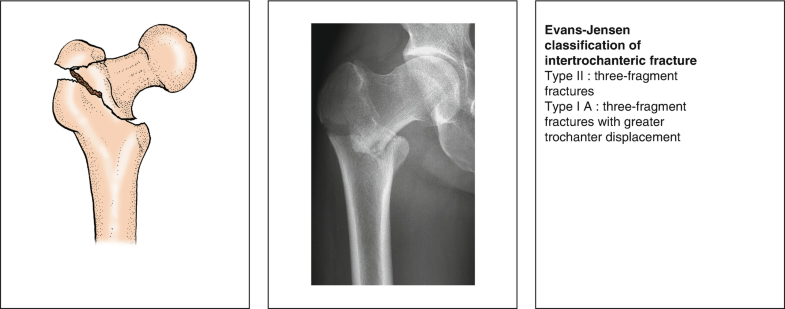
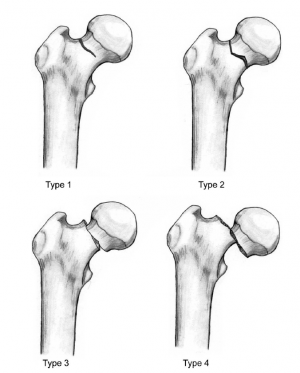
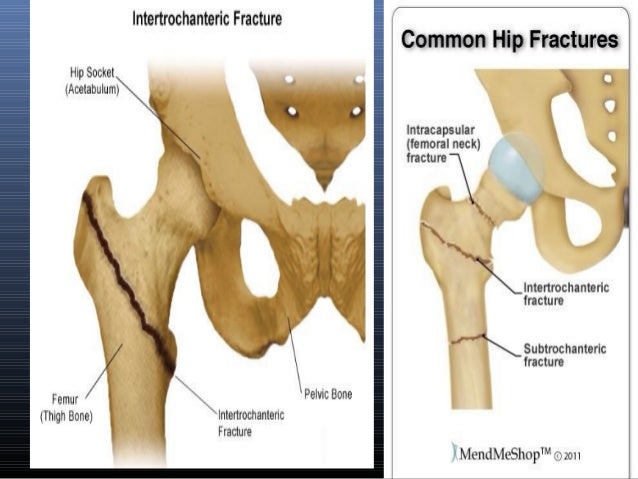
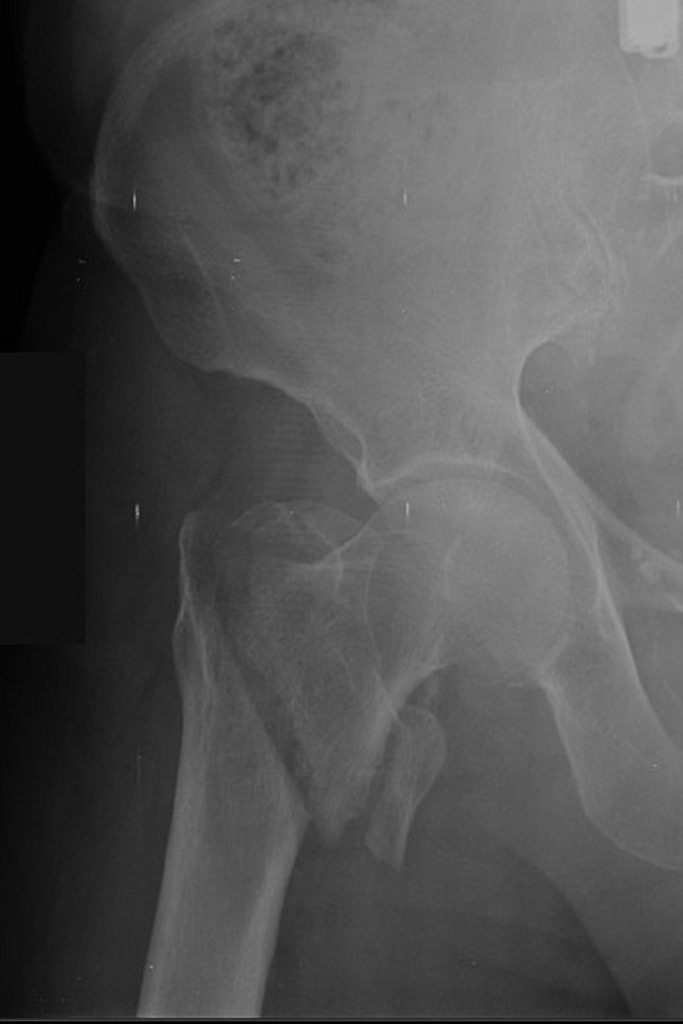
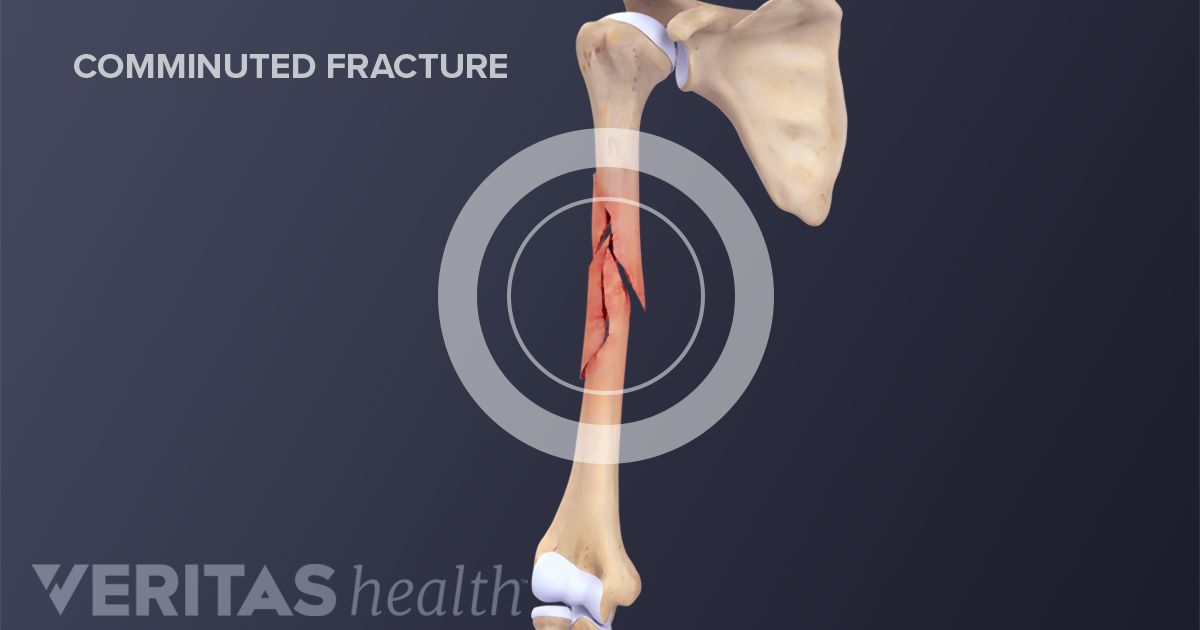
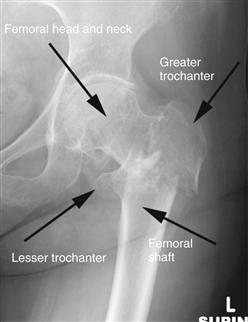
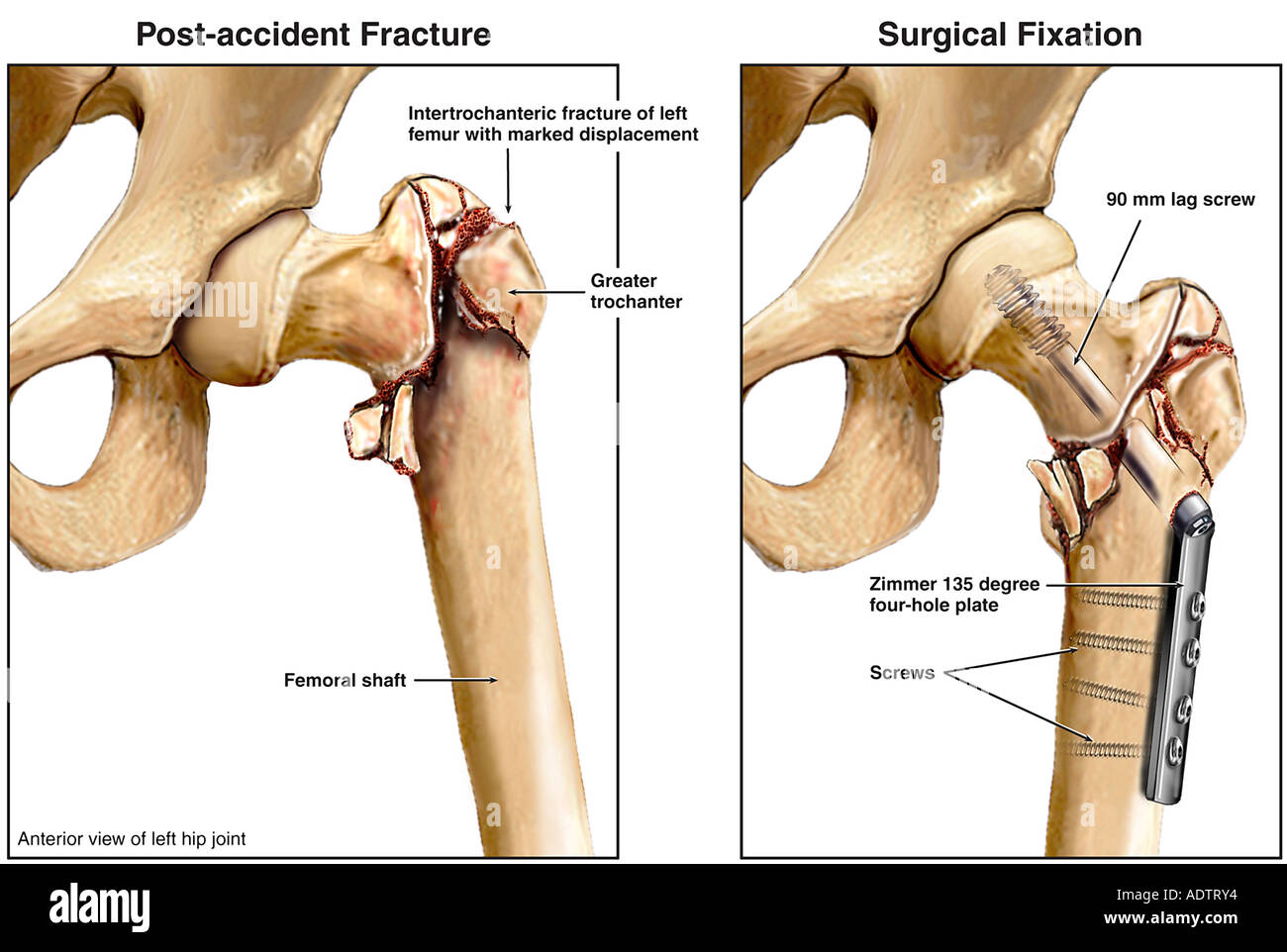
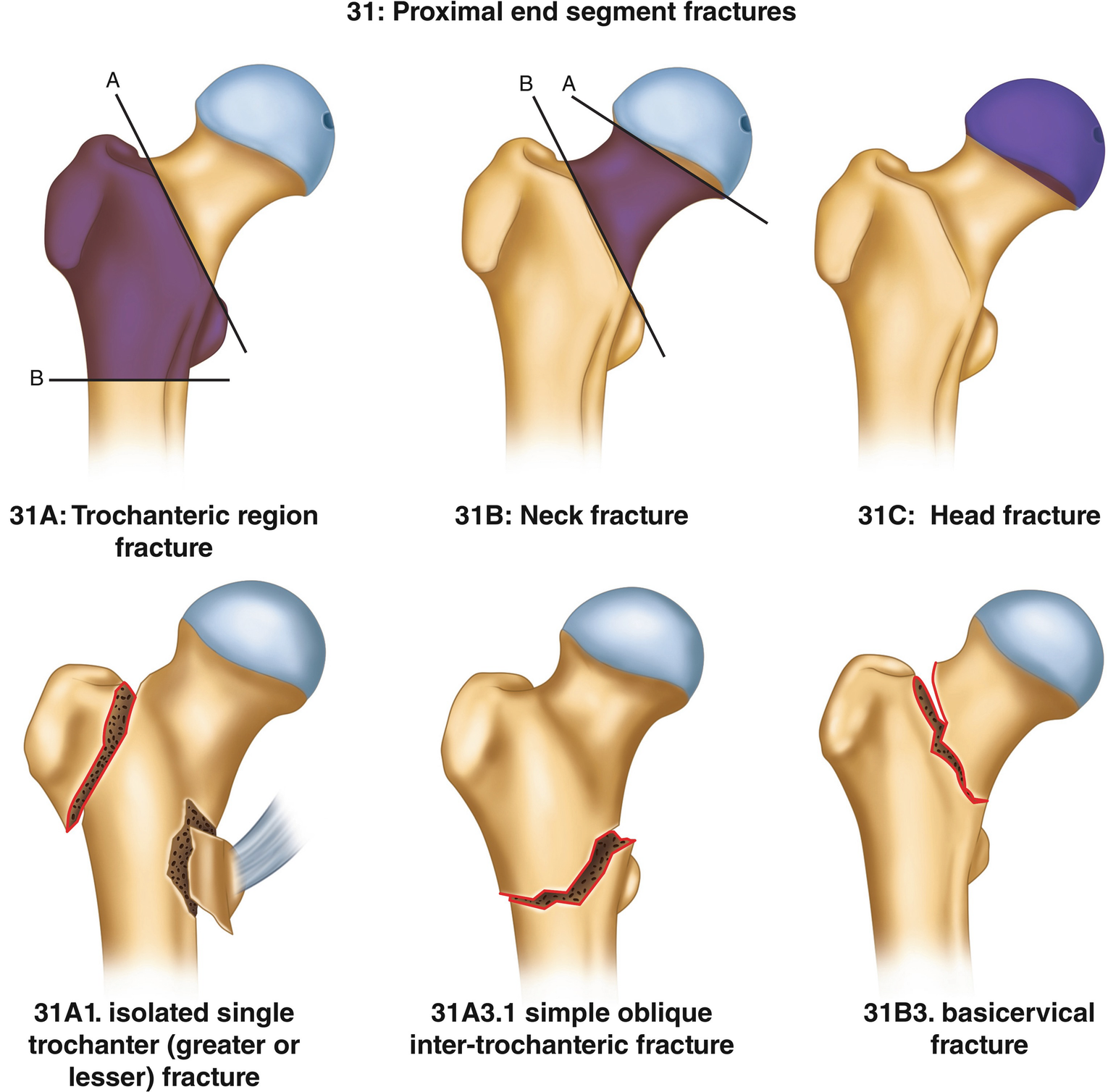
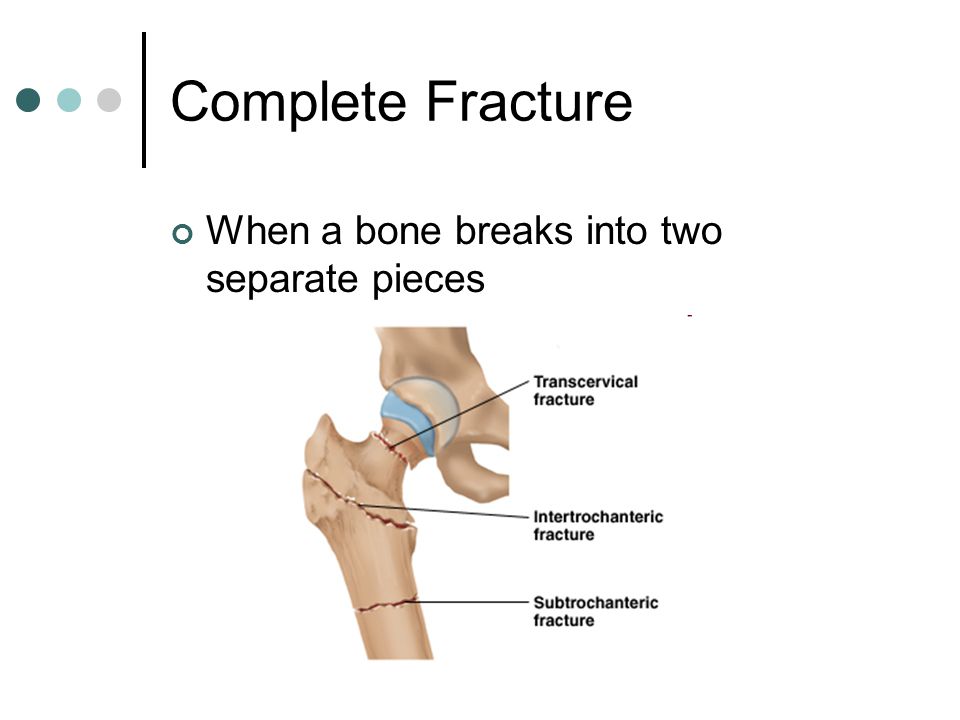
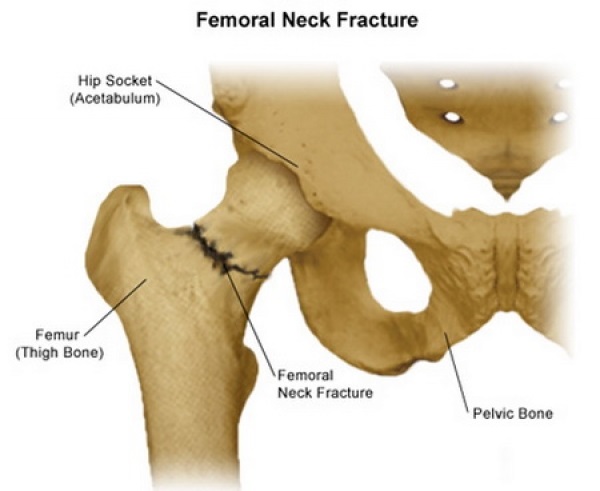 Types of Hip Fractures | Stanford Health Care
Types of Hip Fractures | Stanford Health CareCOVID-19 Update We are experiencing a volume of extremely high calls related to the interest of the COVID-19 vaccine. Please understand that our phone lines should be clear for urgent medical care needs. We cannot accept phone calls to schedule COVID-19 vaccines at this time. When this changes, we will update this website. Please know that our supply of vaccines is extremely small. Read all . Silence Silence Silence I want. .. I want. .. I want. .. Find a doctor Find a doctor at Johns Hopkins Hospital, Johns Hopkins Bayview Medical Center or Johns Hopkins Community Physicians. I want. .. Search Faculty of Research Enter the last name, specialty or keyword for your search below. I want. .. Application for AdmissionFixing Hip Fracturesby Simon Mears, M.D.Introduction Hip fractures are a common injury in the United States; approximately 280,000 occurred in 1998. The number of annual hip fractures is expected to exceed 500,000 per year by 2040. The fracture of a hip can lead to morbidity, a change in life arrangements or death. Mortality rates have been recorded from 12 per cent to 36 per cent. Approximately 22% of patients require a higher level of care 1 year after the hip fracture. Therefore, hip fractures are feared by the elderly. Osteoporosis is characterized by a fragile skeleton resulting from the decrease in bone mass. The predominant mechanism of hip fracture in the larger population is a fall in a standing position People with osteoporosis often have other comorbidities that lead to an increase in the rate of fall. The elderly are also more likely than the general population to experience the type of fall that results in a hip fracture. People with a slower bet have less momentum forward. Therefore, when these people fall, they tend to comb and fall to the side, making a fracture is more likely. The decrease in bone mass in the elderly is due to several factors, including: reduction of the biosynthetic and replicative potential of osteoblasts, increase in osteoclast activity, reduction of physical activity (an stimulation for bone remodeling), genetic predisposition, decrease in calcium intake and hormonal influences. The net result is that bone resorption exceeds the bone building. Postmenopausal women are especially at risk due to estrogen deficiency. Women may lose up to 35% of their cortical bone and 50% of their trabecular bone in 30 to 40 years after menopause. To maintain strength, the cortical bone increases the diameter, but the thickness of the bark decreases. A larger diameter increases the strength of a bone but makes the bone vulnerable to rotary and folding forces. The loss of the trabecular bone, which usually arises along the stress lines, also decreases the strength of the bone. Some people are susceptible to particular injury patterns. Of people who hold a second contralateral hip fracture, 90% experience the same pattern of injury. This finding indicates that microtrabecular architecture should be important. Confirmation methods of the hip fracture In the elderly, hip pain is usually indicative of a fracture. The pain resulting from a fracture usually presents as the beginning of pain of the groin or the upper thigh. Depending on the severity of the injury, the patient may or may not be able to walk. Regardless, a hip fracture, a pelvis fracture, a spinal injury, spinal stenosis, trochanteric bursitis, muscle tears and knee injuries should be ruled out. Anteroposterior pelvis view (AP) allows to compare affected and contralateral hips. The unaffected hip view can be used for preoperative planning. A lateral cross-table X-ray should also be obtained by flexing the unaffected hip and knee and pointing to the X-ray beam on the affected side. This view places the beam at a straight angle towards the femoral neck without manipulating the affected side and reveals any subsequent comminution of the femur. An AP X-ray of the affected hip should be obtained with the leg in internal rotation (see below). At this point of view, the minor trochanter should only be partially visible. The internal rotation view will place the entire neck to better visualize the fracture lines. Because flat X-rays may seem normal or inconclusive, other imaging studies should be considered. Magnetic resonance imaging (MRI) is the most sensitive for the evaluation of fractures, in particular hidden or undisplaced fractures. Magnetic resonance scanners can be used immediately after injury and can reveal soft tissue pathology, such as muscle strains, major trochanteric bursitis and pelvic fractures. Fracture lines immediately after the injury. Edema in soft tissuesThe ossian radionuclide scans that can be used 48 to 72 hours after injury are sensitive to metastatic disease. Bone scans are valuable for patients who cannot get a MRI scan. Computed tomography reveals fractures only when they are displaced. Computed tomographs are useful for detecting the notion of fracture in the presence of hardware. Classification of hip fractures There are three broad categories of hip fractures based on the location of the fracture: , and . Femoral neck fractures The femoral neck is the most common location for a hip fracture, which represents 45% to 53% of the hip fractures. For 100,000 years of person, approximately 27.7 femoral fractures in the neck occur in men and 63.3 occur in women. The femoral neck is the femur region linked by the femoral head proximately and the largest and smaller trochanters in a distally way (which is shown below). A fracture of the femoral neck is intracapsular, which is within the joint of the hip and under the fibrous joint capsule. Although there are other more detailed classification systems, fractures are generally classified as stable and unstable. Each category has different operating management options. Treatment of stable fractures Stable fractures do not move, do not show deformity, or impact on valgus positions. Stable fractures may not be detectable in flat x-rays, and an MRI scan may be required. Because non-cooperative management results in a secondary displacement rate of 40%, stable fractures of the femoral neck are generally treated better with surgical stabilization and immediate mobilization. The treatment is by means of operating fixing with three parallel cannulate screws placed adjacent to the bark of the femoral neck. Treatment of unstable fractures Unstable femoral neck fractures move and can be seen in flat X-rays. In physical examination, the leg of the affected side is rotated externally and shortened; the degree of rotation and shortening varies with the degree of displacement. Displaced fractures in young patients are usually treated with pinning. Pination is chosen because the risks of arthroplasty, including wear and tear, are high for young patients, and their healing rate is high due to the absence of osteoporosis. As age and osteoporosis increases, the rate of failure (notion, secondary displacement, avascular necrosis) increases. Hemi-or total joint arthroplasty is associated with a lower rate of repeat surgery than internal fixation and is often the best choice for older patients. Younger patients may choose to fix screws and rescue hips. In hemiartroplasty, acetabular cartilage remains intact and the joint implant with the acetabulum. Hemiarthroplasty requires less surgery than a total replacement of joints because paracetabulum is not resurmountable. There is a lower risk of dislocation with hemiarthoplasty because it uses a head size much higher than total hip arthroplasty. In more active patients, hemiartroplasty also has a risk of wear of paracetabular cartilage and review of total hip arthroplasty. Femoral implants can be cemented or without cement, and there are many designs of each type. The implantation can be achieved by injection of bone cement around the prosthesis or by bone slowness in the prosthesis. A bipolar implant has two heads so that the movement can occur between one head and the paracetabular cartilage and between the two heads. In theory, this arrangement helps to reduce acetabular wear and to provide an increased movement. A unipolar implant has only one large head that articulates with the paracetabular cartilage. There seems to be no clinical difference between the results of patients with bipolar or unipolar implants in terms of acetabular wear and hip movement. Compared to unipolar implants, bipolar implants are more expensive and have an additional interface for wear prosthesis. Therefore, there does not seem to be a compelling reason to recommend the most expensive bipolar implant on unipolar for the older patient with hip fracture. If the stem is not well fixed on the proximal femur, any of the types will fail quickly. The total replacement of joints is usually performed in an active patient or one with pre-existing arthritis. During a total replacement of joints, the acetabulo is resurfaced and a cup of metal with a polyethylene coating is fixed inside. The hip joint takes place between the head of the implant and the polyethylene coating. The decision to treat femoral fractures of the neck with pinning or arthroplasty is controversial. The advantages of pinning include less invasive surgery, less blood loss and less postoperative morbidity. However, treatment through pining carries a higher risk of more surgery in the future. As implied, arthroplasty results in a more acute postoperative morbidity, but it offers less reoperations for notion, hardware failure and osteonecrosis. My protocol divides patients into three categories: patients with non-displaced fractures, patients with "low" activity with displaced fractures and patients with "high" activity with displaced fractures. Undisplaced fractures are treated with pinning. Displaced fractures in inactive patients are treated with unipolar hemiartroplasty. Displaced fractures in highly active patients are treated with total hip replacement. Treatment failures The screw treatment failures are not late avascular necrosis and bonding. The notion is mainly due to the lack of adequate mechanical stabilization of the fracture. If the bone does not heal, the screws will slide and reverse as the fracture collapses. The nounion typically presents with a worsening of the groin or buttocks. Late avascular necrosis results from insults to blood vessels that supply the neck and femoral head. Radiographic monitoring of up to 3 years should detect most cases of avascular necrosis. Treatment for avascular necrosis or noion is hip replacement. The failure of a hemiarthroplasty causes acetabular pain and erosion. Other complications include dislocation, fracture and infection. Treatment for a failed hemiarthroplasty is conversion to a total hip replacement. The failures of a total hip replacement are similar to that of a hemiartroplasty: loosening, using implants, infection, fracture and dislocation. Treatment for a total hip replacement is a review arthroplasty. Intertrochanter fractures Intertrochanther fractures are ruptures of the femur between the elders and the lower trochanters. They are extracapsular fractures that is, outside the fibrous capsule of the hip joint. The epidemiology of the intertrocatural fractures is similar to that of the femoral fractures of the neck. For 100,000 years, intertrochanteric interruptions occur in 34 men and 63 women. Intertrocatorial fractures represent approximately 38% to 50% of all hip fractures. Many sorting systems, such as the Evans system, have been used to describe intertrocatory hip fractures. However, most systems lack reliability and, in general, intertrocatural fractures can be divided into two categories: stable and unstable. The stable fractures are those in which the femur is divided into two or three parts. Unstable fractures are those in which the femur breaks in four parts or the fracture is of the reverse oblique pattern. Reverse oblique fractures are unstable due to the tendency of the femur to move medianly. This classification method helps to determine which method will be used for fixing. Fractures of two parts have a fracture line through the intertrocatorial zone. While evaluating the stability of a fracture, the most important points to consider are the lateral cusp bone and the greater trochanter and bone on the mid side of the proximal femur called the calcar. Treatment of stable fractures If the fracture is stable, the treatment is with a sliding hip screw coupled to a side plate that is screwed on the femoral axis. (to be shown below) The screw provides proximal fragment fixation. It is established within a telescoping cannon that allows the impact of the bone, which promotes the union of fracture. The lateral dome must be intact so that the screw does not stop sliding. A four-part fracture has several fracture lines. Fractured bone parts include: 1) femoral head, 2) lower trochanter, 3) the largest trochanter, and 4) the remaining femur. Fractures with multiple pieces and fracture lines are called "comminutives". The more pieces, the less stable the fracture pattern. The decrease can make the fixation with a slider hip screw and the most likely side plate that fails. Treatment of Unstable Fractures Approximately 5% of fractures are extremely unstable, and the direction of the fracture is parallel to the femoral neck. This type of fracture is called reverse oblique pattern. A high rate of failure occurs if the fracture is treated with a sliding hip screw and a side plate. Due to the angle of the fracture, there is no bone laterally to stop the slide screw. For unstable intertrocatorial fractures, including those of the reverse oblique pattern and those of subtropical extension, an intramedular hip screw is indicated. This device combines a sliding hip screw with an intramedular nail. There are many patented varieties, including Nail Gamma (Stryker, Mahwah, NJ), Trigen Trochanteric Entry Nail, (TAN uña, Smith and Nephew, Memphis TN) and Nail Femoral Proximal (Synthes, West Chester, PA). Intramedular hip screws can be placed through small incisions, and blood loss can be lower than with a hip screw and sideplate. The nail acts as a metal dome to prevent slide and provides better fixing in unstable fracture patterns. No differences have been found between the two devices in stable fractures. With a short intramedular hip screw, the nail does not extend through the complete shaft of the femur. The cross-lock of the nail is through a jig, which avoids the rotation of the nail inside the femur. Intramedular hip short screws can create an increase in bone stress in the distal screw. With a long intramedular hip screw, the cross lock cannot be done with a jig and must be made free of charge under fluoroscopy. Therefore, the cross-blocking is more difficult. The nail extends across the axis, protecting the rest of the bone from the future fracture. The hip screw should be placed centrally inside the femoral head in the strong subcortical bone. The evaluation of the placement of hip screws is made by determining the tip-apex distance under fluoroscopy. The tip-apex distance is the sum of the distances from the tip of the hip screw to the apex of the femoral head measured on the lateral radiographs and AP Baumgaertner et al. showed that no fracture had loss of secondary fixation for the screw cut when the tip-apex distance was less than 24 mm. When the tip-apex distance was greater than 45 mm, the screw cutting rate increased to 60%. The failure mechanisms of a hip screw include non-union, screw cutting, nail breakage, mesh and limp. Although the slide of the hip screw allows bone compression and hopeful healing, it causes the limb to be shortened and causes weakness of the kidnapping. Most complications are treated with total hip arthroplasty. Subtrochanteric Fractures Subtrocátric fractures are between the lower trocánter and the femoral isthmus, that is, in the proximal part of the femoral axis. They are less common than the femoral neck and intertrocatorial fractures, with an approximate percentage of 5% to 15% of hip fractures. Subtrocatural fractures are less stable than the other two types of hip fractures and, consequently, more difficult to correct. Treatment A subtrocatorial fracture is treated with an intramedullary hip screw. There are no lateral buttocks in a subtrocatorial fracture and therefore the sliding hip screws with side plates provide poor fixation. After surgery for a hip fracture, weight gain should be allowed as tolerated. Patients with less stable fracture patterns have been shown to be protected by weight gain and self-restrictor movement.() Summary In short, the type of fracture determines the type of surgery. Patients with femoral fractures of the neck are treated with pinning or hip arthoplasty, depending on the patient's age and the presence and degree of displacement. Patients with intertrocatorial fractures are treated with a sliding hip screw or an intramedular hip screw, depending on the stability and location of the fracture.() References • Apple DF Jr, Hayes WC, editors. Prevention of drops and hip fractures in the Old. Rosemont (IL): American Academy of Orthopedic Surgeons; 1993.• Baumgaertner MR, Curtin SL, Lindskog DM and Keggi JM. The value of the point-apex distance in predicting the fixing failure of the peritrocatheric fractures of the hip. J Bone Joint Surg 1995;77A(7):1058-1064.• Cummings SR, Rubin SM, Black D. The future of hip fractures in the United States. Numbers, costs and possible effects of postmenopausal estrogen. Clin Orthop Relat Res 1990;252:163-166.• Endo Y, Aharonoff GB, Zuckerman JD, Egol KA, Koval KJ. Gender differences in patients with hip fracture: increased risk of morbidity and mortality in men. J Orthop Trauma 2005 Jan;19(1):29-35.• Koval KJ, DA Room, Kummer FJ, Zuckerman JD. Weight surgery after a fracture of the femoral neck or an intertrocatorial fracture. J Bone Joint Surg 1998; 80A(3):352-356.• Koval KJ, Zuckerman JD. Hip fractures. I: Summaries and assessment and treatment of femoral neck fractures. J Am Acad Orthop Surg 1994;2(3):141-149.• Lofman O, Berglund K, Larsson L, Toss G. Changes in the hip fracture epidemiology: redistribution between ages, genders and types of fracture. Osteoporos Int 2002;13(1):18-25.• Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. The risk of mortality after the hip fracture. J Orthop Trauma 2003;17(1):53-56.• Schroder HM, Petersen KK, Erlandsen M. Occurrence and incidence of the second hip fracture. Clin Orthop Relat Res 1993;289:166-169.()IntroductionOsteoporosis is characterized by a fragile skeleton resulting from the decrease in bone mass. To maintain strength, the cortical bone increases the diameter, but the thickness of the bark decreases. A larger diameter increases the strength of a bone but makes the bone vulnerable to rotary and folding forces. The loss of the trabecular bone, which usually arises along the stress lines, also decreases the strength of the bone. Some people are susceptible to particular injury patterns. Of people who hold a second contralateral hip fracture, 90% experience the same pattern of injury. This finding indicates that microtrabecular architecture should be important. Confirmation methods of the hip fracture In the elderly, hip pain is usually indicative of a fracture. The pain resulting from a fracture usually presents as the beginning of pain of the groin or the upper thigh. Depending on the severity of the injury, the patient may or may not be able to walk. Regardless, a hip fracture, a pelvis fracture, a spinal injury, spinal stenosis, trochanteric bursitis, muscle tears and knee injuries should be ruled out. Anteroposterior pelvis view (AP) allows to compare affected and contralateral hips. The unaffected hip view can be used for preoperative planning. A lateral cross-table X-ray should also be obtained by flexing the unaffected hip and knee and pointing to the X-ray beam on the affected side. This view places the beam at a straight angle towards the femoral neck without manipulating the affected side and reveals any subsequent comminution of the femur. Fracture lines immediately after the injury. Edema in soft tissuesThe ossian radionuclide scans that can be used 48 to 72 hours after injury are sensitive to metastatic disease. Bone scans are valuable for patients who cannot get a MRI scan. Computed tomography reveals fractures only when they are displaced. Computed tomographs are useful for detecting the notion of fracture in the presence of hardware. Classification of hip fractures There are three broad categories of hip fractures based on the location of the fracture: , and . Femoral neck fractures The femoral neck is the most common location for a hip fracture, which represents 45% to 53% of the hip fractures. For 100,000 years of person, approximately 27.7 femoral fractures in the neck occur in men and 63.3 occur in women. The femoral neck is the femur region linked by the femoral head proximately and the largest and smaller trochanters in a distally way (which is shown below). A fracture of the femoral neck is intracapsular, which is within the joint of the hip and under the fibrous joint capsule. Although there are other more detailed classification systems, fractures are generally classified as stable and unstable. Each category has different operating management options. Treatment of stable fractures Stable fractures do not move, do not show deformity, or impact on valgus positions. Stable fractures may not be detectable in flat x-rays, and an MRI scan may be required. Because non-cooperative management results in a secondary displacement rate of 40%, stable fractures of the femoral neck are generally treated better with surgical stabilization and immediate mobilization. The treatment is by means of operating fixing with three parallel cannulate screws placed adjacent to the bark of the femoral neck. Treatment of unstable fractures Unstable femoral neck fractures move and can be seen in flat X-rays. In physical examination, the leg of the affected side is rotated externally and shortened; the degree of rotation and shortening varies with the degree of displacement. Displaced fractures in young patients are usually treated with pinning. Pination is chosen because the risks of arthroplasty, including wear and tear, are high for young patients, and their healing rate is high due to the absence of osteoporosis. As age and osteoporosis increases, the rate of failure (notion, secondary displacement, avascular necrosis) increases. Hemi-or total joint arthroplasty is associated with a lower rate of repeat surgery than internal fixation and is often the best choice for older patients. Younger patients may choose to fix screws and rescue hips. In hemiartroplasty, acetabular cartilage remains intact and the joint implant with the acetabulum. Hemiarthroplasty requires less surgery than a total replacement of joints because paracetabulum is not resurmountable. There is a lower risk of dislocation with hemiarthoplasty because it uses a head size much higher than total hip arthroplasty. In more active patients, hemiartroplasty also has a risk of wear of paracetabular cartilage and review of total hip arthroplasty. Femoral implants can be cemented or without cement, and there are many designs of each type. The implantation can be achieved by injection of bone cement around the prosthesis or by bone slowness in the prosthesis. A bipolar implant has two heads so that the movement can occur between one head and the paracetabular cartilage and between the two heads. In theory, this arrangement helps to reduce acetabular wear and to provide an increased movement. A unipolar implant has only one large head that articulates with the paracetabular cartilage. There seems to be no clinical difference between the results of patients with bipolar or unipolar implants in terms of acetabular wear and hip movement. Compared to unipolar implants, bipolar implants are more expensive and have an additional interface for wear prosthesis. Therefore, there does not seem to be a compelling reason to recommend the most expensive bipolar implant on unipolar for the older patient with hip fracture. If the stem is not well fixed on the proximal femur, any of the types will fail quickly. The total replacement of joints is usually performed in an active patient or one with pre-existing arthritis. During a total replacement of joints, the acetabulo is resurfaced and a cup of metal with a polyethylene coating is fixed inside. The hip joint takes place between the head of the implant and the polyethylene coating. The decision to treat femoral fractures of the neck with pinning or arthroplasty is controversial. The advantages of pinning include less invasive surgery, less blood loss and less postoperative morbidity. However, treatment through pining carries a higher risk of more surgery in the future. As implied, arthroplasty results in a more acute postoperative morbidity, but it offers less reoperations for notion, hardware failure and osteonecrosis. My protocol divides patients into three categories: patients with non-displaced fractures, patients with "low" activity with displaced fractures and patients with "high" activity with displaced fractures. Undisplaced fractures are treated with pinning. Displaced fractures in inactive patients are treated with unipolar hemiartroplasty. Displaced fractures in highly active patients are treated with total hip replacement. Treatment failures The screw treatment failures are not late avascular necrosis and bonding. The notion is mainly due to the lack of adequate mechanical stabilization of the fracture. If the bone does not heal, the screws will slide and reverse as the fracture collapses. The nounion typically presents with a worsening of the groin or buttocks. Late avascular necrosis results from insults to blood vessels that supply the neck and femoral head. Radiographic monitoring of up to 3 years should detect most cases of avascular necrosis. Treatment for avascular necrosis or noion is hip replacement. The failure of a hemiarthroplasty causes acetabular pain and erosion. Other complications include dislocation, fracture and infection. Treatment for a failed hemiarthroplasty is conversion to a total hip replacement. The failures of a total hip replacement are similar to that of a hemiartroplasty: loosening, using implants, infection, fracture and dislocation. Treatment for a total hip replacement is a review arthroplasty. Intertrochanter fractures Intertrochanther fractures are ruptures of the femur between the elders and the lower trochanters. They are extracapsular fractures that is, outside the fibrous capsule of the hip joint. The epidemiology of the intertrocatural fractures is similar to that of the femoral fractures of the neck. For 100,000 years, intertrochanteric interruptions occur in 34 men and 63 women. Intertrocatorial fractures represent approximately 38% to 50% of all hip fractures. Many sorting systems, such as the Evans system, have been used to describe intertrocatory hip fractures. However, most systems lack reliability and, in general, intertrocatural fractures can be divided into two categories: stable and unstable. The stable fractures are those in which the femur is divided into two or three parts. Unstable fractures are those in which the femur breaks in four parts or the fracture is of the reverse oblique pattern. Reverse oblique fractures are unstable due to the tendency of the femur to move medianly. This classification method helps to determine which method will be used for fixing. Fractures of two parts have a fracture line through the intertrocatorial zone. While evaluating the stability of a fracture, the most important points to consider are the lateral cusp bone and the greater trochanter and bone on the mid side of the proximal femur called the calcar. Treatment of stable fractures If the fracture is stable, the treatment is with a sliding hip screw coupled to a side plate that is screwed on the femoral axis. (to be shown below) The screw provides proximal fragment fixation. It is established within a telescoping cannon that allows the impact of the bone, which promotes the union of fracture. The lateral dome must be intact so that the screw does not stop sliding. A four-part fracture has several fracture lines. Fractured bone parts include: 1) femoral head, 2) lower trochanter, 3) the largest trochanter, and 4) the remaining femur. Fractures with multiple pieces and fracture lines are called "comminutives". The more pieces, the less stable the fracture pattern. The decrease can make the fixation with a slider hip screw and the most likely side plate that fails. Treatment of Unstable Fractures Approximately 5% of fractures are extremely unstable, and the direction of the fracture is parallel to the femoral neck. This type of fracture is called reverse oblique pattern. A high rate of failure occurs if the fracture is treated with a sliding hip screw and a side plate. Due to the angle of the fracture, there is no bone laterally to stop the slide screw. For unstable intertrocatorial fractures, including those of the reverse oblique pattern and those of subtropical extension, an intramedular hip screw is indicated. This device combines a sliding hip screw with an intramedular nail. There are many patented varieties, including Nail Gamma (Stryker, Mahwah, NJ), Trigen Trochanteric Entry Nail, (TAN uña, Smith and Nephew, Memphis TN) and Nail Femoral Proximal (Synthes, West Chester, PA). Intramedular hip screws can be placed through small incisions, and blood loss can be lower than with a hip screw and sideplate. The nail acts as a metal dome to prevent slide and provides better fixing in unstable fracture patterns. No differences have been found between the two devices in stable fractures. With a short intramedular hip screw, the nail does not extend through the complete shaft of the femur. The cross-lock of the nail is through a jig, which avoids the rotation of the nail inside the femur. Intramedular hip short screws can create an increase in bone stress in the distal screw. With a long intramedular hip screw, the cross lock cannot be done with a jig and must be made free of charge under fluoroscopy. Therefore, the cross-blocking is more difficult. The nail extends across the axis, protecting the rest of the bone from the future fracture. The hip screw should be placed centrally inside the femoral head in the strong subcortical bone. The evaluation of the placement of hip screws is made by determining the tip-apex distance under fluoroscopy. The tip-apex distance is the sum of the distances from the tip of the hip screw to the apex of the femoral head measured on the lateral radiographs and AP Baumgaertner et al. showed that no fracture had loss of secondary fixation for the screw cut when the tip-apex distance was less than 24 mm. When the tip-apex distance was greater than 45 mm, the screw cutting speed increased to 60%. The failure mechanisms of a hip screw include non-union, screw cutting, nail breakage, mesh and limp. Although the slide of the hip screw allows bone compression and hopeful healing, it causes the limb to be shortened and causes weakness of the kidnapping. Most complications are treated with total hip arthroplasty. Subtrochanteric Fractures Subtrocátric fractures are between the lower trocánter and the femoral isthmus, that is, in the proximal part of the femoral axis. They are less common than the femoral neck and intertrocatorial fractures, with an approximate percentage of 5% to 15% of hip fractures. Subtrocatural fractures are less stable than the other two types of hip fractures and, consequently, more difficult to correct. Treatment A subtrocatorial fracture is treated with an intramedullary hip screw. There are no lateral buttocks in a subtrocatorial fracture and therefore the sliding hip screws with side plates provide poor fixation. After surgery for a hip fracture, weight gain should be allowed as tolerated. Patients with less stable fracture patterns have been shown to be protected by weight gain and self-restrictor movement.() Summary In short, the type of fracture determines the type of surgery. Patients with femoral fractures of the neck are treated with pinning or hip arthoplasty, depending on the patient's age and the presence and degree of displacement. Patients with intertrocatorial fractures are treated with a sliding hip screw or an intramedular hip screw, depending on the stability and location of the fracture.() References • Apple DF Jr, Hayes WC, editors. Prevention of drops and hip fractures in the Old. Rosemont (IL): American Academy of Orthopedic Surgeons; 1993.• Baumgaertner MR, Curtin SL, Lindskog DM and Keggi JM. The value of the point-apex distance in predicting the fixing failure of the peritrocatheric fractures of the hip. J Bone Joint Surg 1995;77A(7):1058-1064.• Cummings SR, Rubin SM, Black D. The future of hip fractures in the United States. Numbers, costs and possible effects of postmenopausal estrogen. Clin Orthop Relat Res 1990;252:163-166.• Endo Y, Aharonoff GB, Zuckerman JD, Egol KA, Koval KJ. Gender differences in patients with hip fracture: increased risk of morbidity and mortality in men. J Orthop Trauma 2005 Jan;19(1):29-35.• Koval KJ, DA Room, Kummer FJ, Zuckerman JD. Weight surgery after a fracture of the femoral neck or an intertrocatorial fracture. J Bone Joint Surg 1998; 80A(3):352-356.• Koval KJ, Zuckerman JD. Hip fractures. I: Summaries and assessment and treatment of femoral neck fractures. J Am Acad Orthop Surg 1994;2(3):141-149.• Lofman O, Berglund K, Larsson L, Toss G. Changes in the hip fracture epidemiology: redistribution between ages, genders and types of fracture. Osteoporos Int 2002;13(1):18-25.• Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. The risk of mortality after the hip fracture. J Orthop Trauma 2003;17(1):53-56.• Schroder HM, Petersen KK, Erlandsen M. Occurrence and incidence of the second hip fracture. Clin Orthop Relat Res 1993;289:166-169.()Request an AppointmentTagient Care410-550-0925 Is he already a patient? Traveling for Care? Whether you are crossing the country or the globe, we facilitate access to world-class attention in Johns Hopkins. Outside Maryland (free)410-464-6713International Patients+1-410-502-7683Next Johns Hopkins MedicineContact Information or Find a .News & Policies(Patients & Health Plan Members)Assistance of languages available: © Johns Hopkins University, Johns Hopkins Hospital and Johns Hopkins Health System. All rights reserved.

Treatment of intertrochanteric fracture femur by Ilizarov fixator in elderly patients Ghoneem HF, Zayda AI, Ali El Sayed AF - Menoufia Med J
Subtrochanteric Fractures | SpringerLink

Products – Stock Trial Exhibits
Classification of Femoral Fractures | SpringerLink
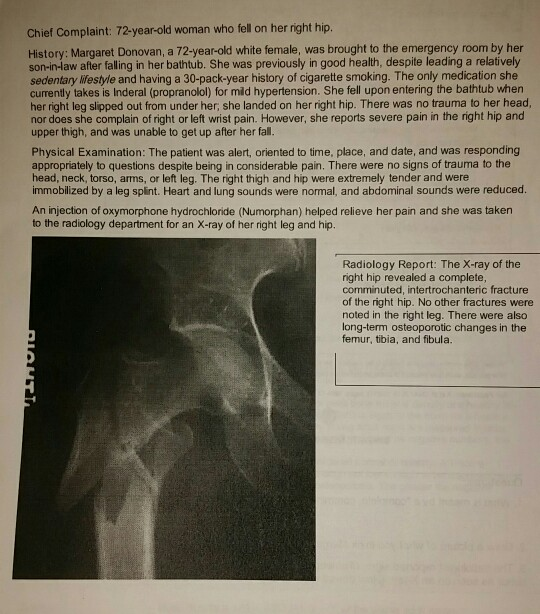
Solved: Chief Complaint: 72-year-old Woman Who Fell On Her... | Chegg.com
Atypical Femoral Fractures

Intertrochanteric Femur Fracture Classification | eORIF
Hip Fracture - Physiopedia

The effectiveness of primary bipolar arthroplasty in treatment of unstable intertrochanteric fractures in elderly patients | Request PDF

Intertrochanteric Fractures : Wheeless' Textbook of Orthopaedics

Intertrochanteric Fractures - Trauma - Orthobullets
Intertrochanteric fracture
Comminuted intertrochanteric fracture | Radiology Case | Radiopaedia.org

Hip fractures - AMBOSS
Comminuted Fracture Definition | Back Pain and Neck Pain Medical Glossary

Proximal femoral fracture
Intertrochanteric Fractures | Musculoskeletal Key

Hip Fracture High Resolution Stock Photography and Images - Alamy

Proximal Femoral Fractures: What the Orthopedic Surgeon Wants to Know | RadioGraphics

Acute comminuted intertrochanteric hip fracture - JETem
Intertrochanteric High Resolution Stock Photography and Images - Alamy
Femur | SpringerLink
Preliminary experience with EBA ONE intramedullary nail for the treatment of pertrochanteric fractures
Fragility fractures of the proximal femur: review and update for radiologists

78 year-old female injured her right hip fracture by fall. (A) Initial... | Download Scientific Diagram

Radiology Report The X ray of the right hip revealed a complete comminuted | Course Hero
Fractures, Sprains, and Dislocations - ppt video online download

Intertrochanteric Fractures Causes, Presentation and Treatment | Bone and Spine

Intertrochanteric Hip Fractures - Everything You Need To Know - Dr. Nabil Ebraheim - YouTube

Intertrochanteric femur fracture - WikEM
Intertrochanteric Fractures | Musculoskeletal Key

Fixing Hip Fractures

Intertrochanteric Hip Fractures | Radiology Key
Learning Radiology - Fractures of the Proximal Femur
Emergency Radiology - Trauma (Comminuted intertrochanteric fracture - Plain film, Radiograph)

Garden classification of hip fractures | Radiology Reference Article | Radiopaedia.org

Treatment of recent trochanteric fracture in adults - ScienceDirect
Fracture After Total Hip Replacement - OrthoInfo - AAOS

Proximal Femoral Fractures: What the Orthopedic Surgeon Wants to Know | RadioGraphics
Classifications of Intertrochanteric fractures and their Clinical Importance
Posting Komentar untuk "complete comminuted intertrochanteric fracture"